INTRODUCTION
Scleral lens is a large-diameter, gas-permeable contact lens that rests on the bulbar conjunctiva, covering the sclera and vaulting the entire cornea and the limbus.1 This vaulting generates a space between the cornea and the scleral lens, filled with preservative-free fluid to form the fluid reservoir.1 The scleral lens can be fluid-ventilated, in which the lens is fitted with minimal or no tear exchange, or fenestrated, in which the lens is fitted with a hole in the transition zone of the scleral lens. The scleral lenses are indicated for various ocular conditions majorly categorized as irregular corneas, refractive errors, ocular surface disorders, and lid/orbit disorders.2 Irregular corneas include primary corneal ectasia, post-keratoplasty, post–refractive surgery, corneal scarring, and post–traumatic surgeries.2 Rigid gas-permeable lenses have shown significant vision improvement in posttraumatic cases compared with manifest spectacle correction.3 The primary refractive complications due to ocular trauma are irregular astigmatism and high-hypermetropia post–traumatic cataract removal.4 The fluid reservoir of the scleral lens creates a suitable optical surface that masks surface irregularity and corneal astigmatism, resulting in improved vision.5 A retrospective study reported that fluid-ventilated scleral lenses were fitted to the pediatric population, with ages ranging from 7 months to 13 years. In this study, scleral lenses were primarily fitted for ocular surface disorders (87%) and only 13% were attributed to refractive errors.6 Few studies have reported the importance of fitting fluid-ventilated scleral lenses in this young age group to correct refractive errors and avoid amblyopia. Meanwhile, these studies have highlighted the challenges associated with fitting evaluation, insertion, and removal training for parents.6,7 This case report describes the novel refractive management of the open globe penetrating injury in a pediatric case using a fenestrated scleral contact lens. No identifiable health information was included in this case report.
CASE REPORT
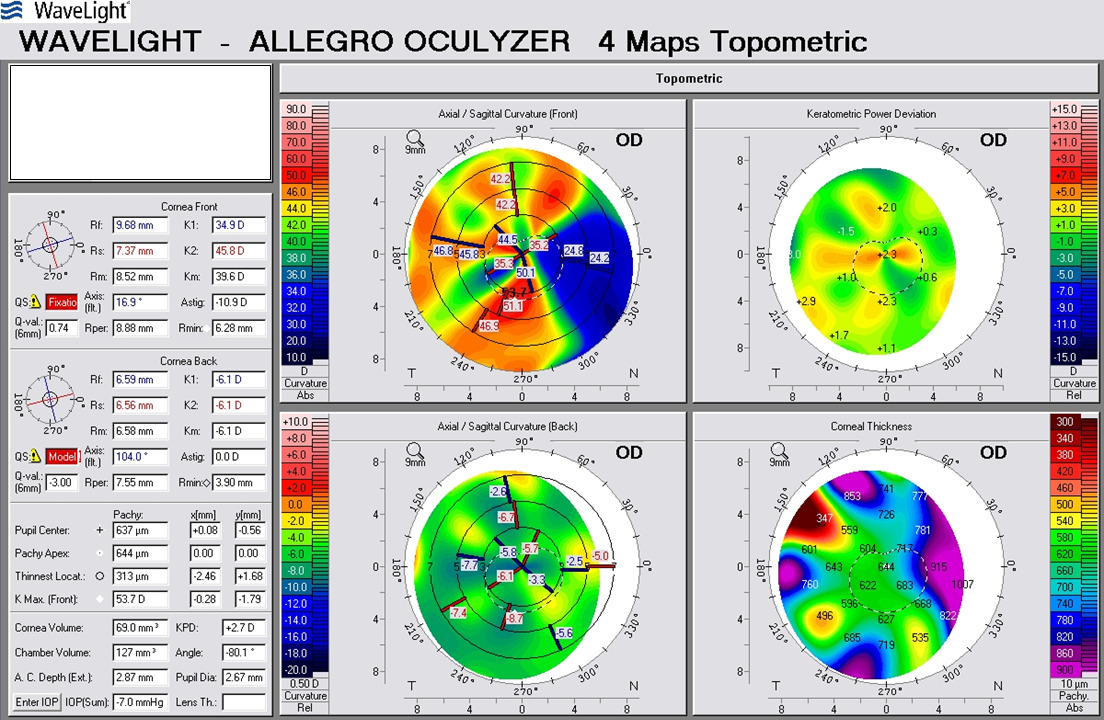
A boy aged 3 years presented to the emergency department of a tertiary eye care centre in India with complaints of pain, redness, watering, and bleeding from the right eye. Parents reported that the child encountered a fall from the cot of a 3-foot height 2 hours before and landed on the metal rod creating severe damage to the right eye. A preliminary slit lamp biomicroscopy examination in the emergency department revealed a nasal limbal scleral tear with iris prolapse (Figure 1A). Visual acuity was recorded as a positive response to the perception of light with accurate responses for the projection of rays from different gazes in the right eye. The B-scan ultrasonography was performed to evaluate the posterior segment, which revealed a clear crystalline lens with the echo of the posterior lens capsule, a clear vitreous with a fully attached retina in all the quadrants, and the absence of any foreign body. Subsequently, the child underwent scleral tear repair on the same day under general anaesthesia. Healing was well appreciated in the follow-up visits (Figure 1B), and the objective refraction with retinoscopy showed a significantly high irregular astigmatism of approximately 10 diopter in the right eye and +0.50 diopter sphere in the left eye. The corneal topography was performed using Allegro Oculyzer (WaveLight, Germany) to clinically correlate with the objective refraction to decide on the astigmatism correction (Figure 2). The customized soft toric contact lens did not show a satisfactory improvement in visual acuity (1.80 converted to logMAR from Teller Acuity Card), whereas the corneal gas-permeable lens improved the visual acuity to 1.10 logMAR (converted). Though there was a clinically significant improvement in visual acuity, the child was symptomatic with the corneal gas-permeable lens. As a result, the child was shifted to the scleral lens to ensure better compliance than the corneal gas-permeable lens. The child was fitted with a BostonSight Prosthetic Replacement of the Ocular Surface Ecosystem lens of 16.00 mm diameter, 7.90 mm base curve and a 3.00 mm sag (Figure 3A). The overrefraction was performed by the same examiner and most of the corneal astigmatism was corrected by the scleral lens. The visual acuity improved from 1.80 logMAR (unaided) to 1.10 (scleral lens) in the right eye. The scleral lens fitting assessment showed acceptable fitting characteristics with no lens movement, no midhaptic compression, no edge lift, no impingement, and no visible turbidity change in the fluid reservoir with adequate vault after 6 hours of scleral lens wear. On removal, excessive negative suction was felt with the lens after 6 hours of scleral lens wear.
Moreover, parents were also concerned about the insertion and removal techniques. So, they were given training to insert the scleral lens by swaddling the child and maintaining the head posture to minimize the attempts, but the child was uncooperative. Finally, the case was managed with a BostonSight Prosthetic Replacement of the Ocular Surface Ecosystem lens, with single fenestration made on the limbal area at 4 o’clock positioning (Figure 3B).
The fenestrated scleral lens showed a similar visual acuity and the haptic alignment of the previous nonfenestrated lens. The central vault was modified to maintain the fluid reservoir thickness to 150 microns with adequate limbal fluid reservoir thickness. The air bubble formed due to fenestration was not obscuring the visual axis and also did not leave any corneal or limbal staining on removal after 6 hours of scleral lens wear. Parents also reported that the insertion of a fenestrated scleral lens was easier compared with the nonfenestrated lens.
The fenestrated scleral lens was dispensed 4 months after the ocular injury in the right eye, and the best corrected visual acuity with the fenestrated scleral lens was improved to 1.10 logMAR. The child was advised to undergo amblyopia patching therapy for 3 to 4 hours per day with the fenestrated scleral lens on the right eye. For amblyopia patching therapy, the child was provided with a 3M Opticlude eye patch, and the child did not show any skin allergic reaction. The parents were advised to engage the child in near activities by patching the left eye and using the fenestrated scleral lens on the right eye under their guidance.
At the 3-month follow-up visit, the history revealed that the child was regularly following the amblyopia patching therapy with the fenestrated scleral lens on the right eye and was compliant with the lens. The parents also reported that the lens was worn for almost 10 to 12 hours a day, with 1 or 2 sleep breaks in between, and was removed during sleep. They also mentioned a change in the child’s behavior, of being calm and comfortable immediately after lens application in recent days compared with the initial 1 to 2 weeks following lens dispensing. There were no signs of discomfort during or at the end of the day with scleral lens wear. The fenestrated scleral lens fitting characteristics showed no changes compared with the previous visit and the visual acuity showed an improvement to 0.80 logMAR in the right eye with fenestrated scleral lens. A few scratches and deposits were noted in the transition zone. An additional cleaner was suggested to use with the existing multipurpose solution. The patient was advised to continue the amblyopia patching therapy and have a regular follow-up once in 6 months.
DISCUSSION
In recent years, the scleral lens practice in India started emerging with better utilization of locally available resources and adaptation to evidence-based practice. This case report demonstrates the benefit of fitting a fenestrated scleral lens for visual rehabilitation in the case of pediatric open globe injury. A retrospective study that reviewed the post–open globe injury cases reported that 97% of patients showed 2 to 3 lines of improvement with the contact lenses, compared with the manifest refraction, irrespective of the prescribed contact lens type.3 The soft contact lens was mostly considered for surgical aphakia and the rigid gas-permeable lens in cases of other open globe tear repair, which induces astigmatism.3 Though the soft lens offers greater comfort and compliance, it did not aid the vision improvement in this case. So, the corneal gas-permeable lens was tried to compensate for the induced corneal astigmatism due to scleral tear repair. The corneal gas-permeable lens showed a clinically significant vision improvement, but it was not dispensed considering various factors, including the patient’s symptoms with the lens, compliance, and dislocation of the lens. In a previous study,8 the author reported that approximately 85% of the pediatric population was fitted with corneal gas-permeable lenses and reported only 5% to 6% of patients had corneal gas-permeable lens intolerance, but approximately 80% of the sample population was in the age group of younger than 12 months. Children in the younger age group have a better tolerance to contact lenses compared with the other age group,8 and the practitioner can control the eye rubbing actions using hypoallergic protective goggles with a headband; but in this case, the child was old enough to take off the spectacle. To overcome the patient’s symptom with the corneal gas-permeable lens, the child was fitted with the fluid-ventilated scleral lens by the clinician maintaining the optimal central and limbal fluid reservoir thickness, with good haptics showing no blanching, impingement, or edge lift. The previous study suggested that the optimum central and limbal fluid reservoir thickness should be maintained at approximately 200 to 400 microns and 100 to 200 microns, respectively, with no obstruction of blood vessels and well-aligned edges.9 However, the application was difficult even for the trained professional as the child was uncooperative. The parents were more concerned about the insertion and removal of the fluid-ventilated scleral lens, so they were given training by swaddling the child and maintaining the head posture toward the ground for insertion. They were able to insert the lens somehow, but the bubble formation persisted in all the attempts because of the saline spill as the parents were not able to control the resistance of the child. After multiple attempts, the parents reported difficulty in lens application and difficulty in reinsertion because of the bubble formation; moreover, the recent study highlighted that approximately 35% of scleral lens discontinuation was due to handling issues.10 For easy administration and better compliance, the child was fitted with the fenestrated scleral lens as it is not necessary to fill the bowl with preservative-free fluid, does not require the patient’s head to be facing downwards, and does not need tight hold and wide opening of eyelids, which are required for inserting the fluid-ventilated scleral lens.11 Moreover, the removal of fenestrated scleral lenses does not require a suction cup. The fenestrated scleral lens also has various advantages, including the release of lens suction, reduced fluid reservoir turbidity due to constant exchange of tears, and reduced corneal edema.11 Though the fenestrated scleral lens has more clinical benefits, it also has its disadvantages, of which there is a possibility of corneal desiccation due to the large bubble staying inside the fluid reservoir and fitting challenges while controlling the bubble.11 But in this case, no corneal staining was noted after 6 hours of fenestrated scleral lens wear in the clinics at the first visit and after 3 months of follow-up with adequate central and limbal fluid reservoir thickness.
Usually, eye injuries are classified using two systems: (1) the Birmingham Eye Trauma Terminology classification based on the type and the place of insult and (2) the Ocular Trauma Classification Group based on the extent of the injury. According to the classifications, the child had an open globe penetrating injury in zone 2 of the area no more than 5 mm from the corneoscleral limbus. A previous study3 reported that the presenting visual acuity in patients with ocular open-globe injury involving zone 2 ranges from 1.3 to 3.0 logMAR, whereas in the present case, the visual acuity was positive perception of light with accurate identification of projection of rays from different gazes. The same study3 also highlighted the significant visual acuity improvement in posttraumatic events with contact lenses ranging from 0.0 to 0.6 logMAR, whereas in the present case, the visual acuity with fenestrated scleral lens improved to 1.10 logMAR (converted). This reduction in vision could be because of refractive amblyopia as there was no clear visual stimulation for approximately 4 months posttrauma during the visual system development stage. Though the crucial cornea or the visual axis was not directly involved in the injury, significant topographic changes were noted because of the scleral tear repair. These topographic changes induced approximately 10 dioptres of cylinder and iris prolapse, which resulted in vision deprivation. The amblyopia could not be ruled out in this case as it was unilateral involvement with high astigmatic refractive error in the actively developing visual system and the structural abnormality was not in proportion to the visual deprivation with the fenestrated scleral lens. In the follow-up visit, the visual acuity improved to 0.80 logMAR (converted), which was believed to be the effect of the combination therapy of optical correction with fenestrated scleral lens and amblyopia patching therapy. The child showed an improvement of 3 lines in visual acuity after 12 weeks of combination therapy, which is in accordance with the study reporting a mean improvement of 3.6 lines in visual acuity in the case of children with severe amblyopia after 17 weeks of 2-hour patching therapy.12 Moreover, the age of the child played a key role in this case whether it was the vision deprivation or the vision improvement because of visual system adaptation in the “critical period” of visual development until the age of 6 to 7 years.13 The combined therapy was advised to continue in the follow-up visit by considering the age for further improvement in vision.
To the extent of the authors’ knowledge, this is the first case to be reported from India managing an open globe injury in a child aged 3 years with the fenestrated scleral lens. At a young age, clear visual perception is required for the proper development of the visual system. The refractive error affecting the image formation should be corrected to the maximum as early as possible to reduce this type of amblyopic change in growing children. The fenestrated scleral lens is considered better optical management in the case of pediatric open globe injury.
CONCLUSION
The fenestrated scleral lens served as a refractive aid for the irregular corneal astigmatism caused by the scleral tear repair post–open globe injury. Moreover, the fenestrated scleral lens can be considered as an option in cases of intolerance to the corneal gas-permeable lenses. It also addressed the important challenge of complexity in lens insertion and removal when fitted with the fluid-ventilated scleral lens in the pediatric population.
TAKE HOME POINTS
-
Scleral lenses can be considered in the pediatric population due to their potential poor acceptance of corneal gas-permeable lenses.
-
The application of fenestrated scleral lenses is relatively easier compared to fluid-ventilated scleral lenses.
-
Optimal refractive correction is crucial in the pediatric population, as the visual system is vulnerable to any deprivation of visual stimuli.
Financial support and sponsorship
This case report was supported by the Hyderabad Eye Institute and the Hyderabad Eye Research Foundation.

_nasal_scleral_tear_with_iris_prolapse_and_(b)_p.jpeg)
_right_eye_fitted_with_fluid-ventilated_prose_an.jpeg)
_nasal_scleral_tear_with_iris_prolapse_and_(b)_p.jpeg)
_right_eye_fitted_with_fluid-ventilated_prose_an.jpeg)