INTRODUCTION
Fuchs endothelial corneal dystrophy is the most common endothelial dystrophy and is a leading cause of corneal transplantation. In addition to endothelial keratoplasties that require donor graft tissue such as Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty, another option for patients with Fuchs dystrophy includes descemetorhexis without endothelial keratoplasty, which is also known as Descemet stripping only. Fuchs dystrophy can sometimes limit the ability to predict cataract surgery outcomes as all lens calculations are based on normal eyes without corneal pathology. Additionally, endothelial keratoplasty can change the refraction by at least 0.5 diopter. In these cases with corneal pathology, using a light adjustable lens (RxSight, Aliso Viejo, California) may be helpful. A light delivery device can be used after cataract surgery to change the shape of light adjustable intraocular lenses and thereby change the patient’s prescription to the desired result. This case shares an important example of a patient with Fuchs dystrophy and cataract who was successfully treated with combined Descemet stripping only and light adjustable lens implantation surgeries.
CASE REPORT
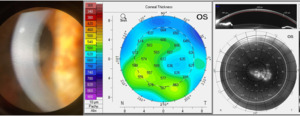
A 58-year-old male patient with a history of prior myopic laser-assisted in situ keratomileusis in the right eye presented seeking spectacle independence. He was happy with his uncorrected distance visual acuity of 20/30 in the right and left eyes but desired better reading vision. His uncorrected near visual acuity was 20/50+2 in the right eye and 20/50-2 in the left eye. He could see 20/40-2 with both eyes. His refractive error and best-corrected visual acuity of the right eye was +1.25 diopter sphere 20/20 and left eye +0.50 -0.25 x090 20/30-2. Corneal examination showed Fuchs dystrophy in both eyes, with prominent 2+ guttata centrally in both eyes and 2+ paracentral edema in the left eye. The patient’s central endothelial cell density was unable to be obtained owing to his central Fuchs dystrophy, but his paracentral endothelial cell density was relatively normal with 3,118 cells/mm2 and 2,754 cells/mm2; however, the asymmetry was suggestive of worse endothelial dysfunction in the left eye. Central pachymetry also showed thicker-than-average corneas and asymmetry between the eyes with corneal thickening of 570 µm in the right eye and 606 µm in the left eye (see Figure 1 for preoperative appearance). The patient also had trace nuclear sclerotic cataracts in both eyes.
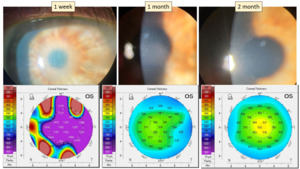
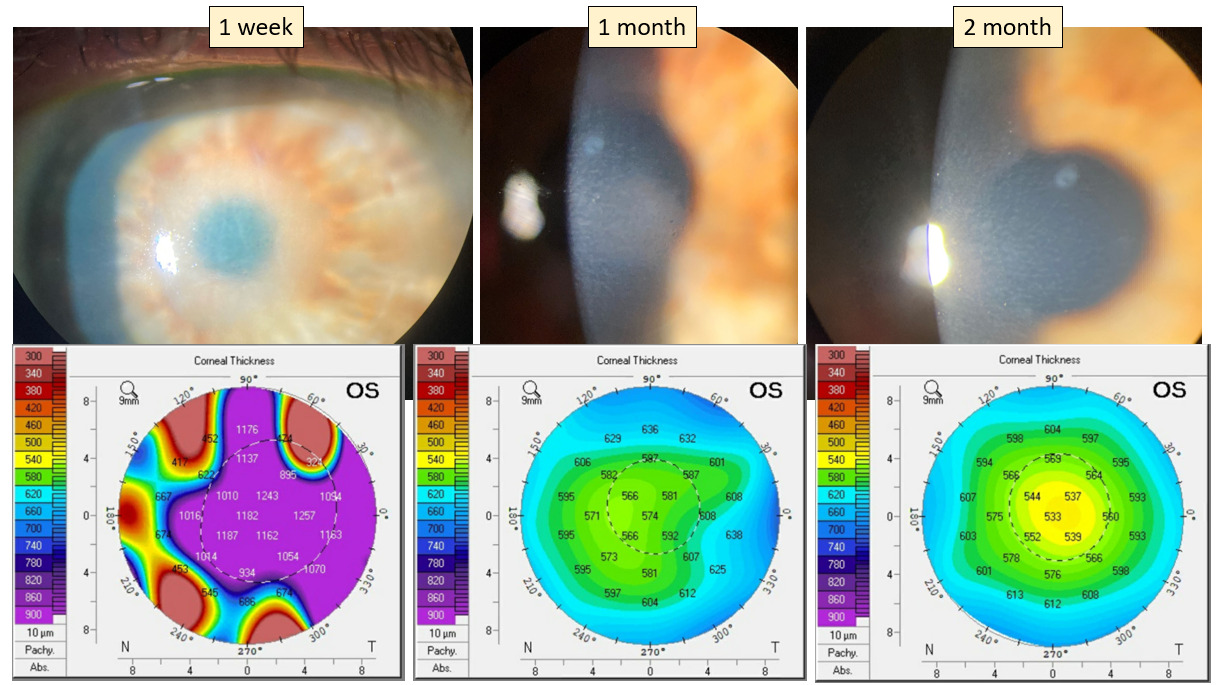
The patient’s primary goal for surgery was to improve his refractive outcome, but laser-assisted in situ keratomileusis is contraindicated in Fuchs dystrophy and photorefractive keratectomy is not ideal for patients with visually significant Fuchs dystrophy and early cataracts. The patient therefore underwent Descemet stripping only and refractive lens exchange phacoemulsification with implantation of a light adjustable lens in the left eye and an aim of -1.00 diopter sphere. The Barrett Universal Formula was used for the lens calculations. At 1-day postoperative examination, his vision was 20/200 in the left eye. On examination, a 5-mm round, 3+ central microcystic corneal edema in the area of the Descemet membrane and endothelium removal was noted. One week postoperatively, significant corneal edema was still observed with stable acuity of 20/200. Pachymetry was 1,182 µm in the left eye. The patient used a Rho-kinase inhibitor ripasudil 0.4% (Glanatec) four times a day to help stimulate endothelial cell migration from the peripheral cornea to the central cornea. This process of endothelial cell migration takes several months, and Rho-kinase inhibitors can speed up the process. He also used a hypertonic sodium chloride solution twice a day to help with corneal deturgescence and prednisolone acetate 1% four times a day to decrease corneal inflammation.
At 1 month, his uncorrected distance visual acuity in the left eye was 20/25-3. His best-corrected distance visual acuity was 20/20-2 with Plano -0.25 x090 refraction. A 2-mm circle of corneal edema persisted at this point. Pachymetry was 574 µm in the left eye, which was a significant reduction from the month prior. Endothelial cell density was unable to be obtained at this visit owing to corneal edema.
At the 2-month follow-up, his uncorrected distance visual acuity in the left eye was 20/20-1 and 20/20 with both eyes. The cornea was clear without edema at this point. Central corneal pachymetry was 533 µm. The cornea was finally clear enough at this point to obtain specular microscopy, which showed central endothelial cell density was 2,486 cells/mm2 (see Figure 2 for 1-week, 1-month, and 2-month postoperative appearance).
At the 3-month follow-up, the patient’s cornea was healed and his refraction was stable in the left eye with -0.25 diopter sphere. The patient’s light adjustable intraocular lens was treated with the light delivery device. The patient’s target goal was set for -1.50 diopter sphere, and following one successful treatment, he refracted very near the target with a refractive outcome of -1.50 -0.25 x180. Patients can have up to three treatments to change the prescription of this monofocal lens by up to 2 diopters of sphere and/or cylinder power. This patient only needed one treatment, which then was followed by two additional lock-in procedures, thereby finalizing his prescription with monovision near in the left eye as desired and preventing any further changes to the lens with ultraviolet light. At each light adjustment, the patient must be fully dilated, and the treatment takes anywhere between 30 and 120 seconds (see Figure 3 for 4-month postoperative appearance).
At the final follow-up 9 months after surgery, the patient’s uncorrected distance visual acuity in the left eye was 20/30. Best-corrected distance visual acuity was 20/20 with a refraction of -1.00 diopter sphere. It is possible this slight change in refractive error may be accounted for by a hyperopic shift after Descemet stripping only or from variability among examiners. The patient was still very satisfied with his uncorrected near visual acuity of 20/25 in the left eye. Binocular uncorrected distance visual acuity was 20/20-2 and binocular uncorrected near visual acuity was 20/25. The patient’s endothelial cell count remained stable at 2,299 cells/mm2. Stereopsis showed suppression of the patient’s right eye with negative stereopsis, but the patient did not report any challenges with depth perception. He denied experiencing symptoms of aniseikonia. Log contrast sensitivity in full illumination was measured to be 1.16 right eye, 1.28 left eye, and 1.56 both eyes, and in dark illumination was measured to be 1.12 right eye, 1.36 left eye, and 1.44 both eyes. It is presumed that the cause for the reduction in contrast sensitivity of the nonoperative right eye was because that eye still had a cataract and Fuchs dystrophy. The patient reported excellent vision and was very satisfied, and the left eye has remained stable since.
DISCUSSION
A patient with presbyopia desiring to be independent from contact lenses and glasses has several options. In the United States, in addition to corneal refractive surgery such as laser-assisted in situ keratomileusis and photorefractive keratectomy, lens-based surgery is an effective way to treat presbyopia.1 Although laser-assisted in situ keratomileusis is contraindicated in patients with Fuchs dystrophy,2 lens-based surgery combined with endothelial surgery can have great refractive outcomes. Different intraocular lenses have been developed to decrease spectacle dependence. Multifocal intraocular lenses, extended-depth-of-focus intraocular lenses, and accommodating intraocular lenses have all been used to increase the range of useful vision. Besides using one of these lenses, monovision or blended vision, where one eye is used more for distance and the other is used more for near vision, has been successfully used for years.3,4 The trade-offs between these different modalities include decreased quality of vision with multifocal lenses and decreased range in extended-depth-of-focus lenses.5,6 Fuchs endothelial dystrophy also has a negative impact on contrast sensitivity.7 The currently available accommodating lenses in the United States have variable predictability and can be an issue if future endothelial surgery is needed. Accommodating lenses are designed to move inside the eye. During endothelial keratoplasty, the anterior chamber is frequently shallowed, which can lead to a change in position in accommodating lenses.
With monovison or blended vision, the difference between the two eyes may be difficult for patients to get used to. Although some have reported decreased stereo vision in patients with monovision, using blended vision instead can lead to good stereoacuity in some cases.8 All of the above technologies can take time to get used to, but blended vision has a reported acceptance rate of 97% at 1 year.9 The additional difficulty in our patient was the corneal pathology, which needed to be addressed for the patient to improve his vision. Any patient with corneal pathology is at an increased risk of future surgery; thus, consideration must be given that any lens choice does not limit or have a negative effect on future surgery. Given the limitations outlined above, a multifocal lens was not deemed a good choice. Although Descemet stripping only has only been used for a few years for a subset of patients, it has become a viable technique for the treatment of Fuchs dystrophy, achieving good visual acuity and a clear cornea.10 Descemet stripping only does not require the use of donor graft tissue, as would be necessary with other keratoplasties such as Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Inhibition of Rho-associated kinase with Rho-kinase inhibitors such as ripasudil is often performed after Descemet stripping only procedures, as Rho-kinase inhibitors have been reported to have a stimulatory effect on corneal endothelial cell migration and may enhance a patient’s recovery.11
Descemet stripping only surgery has the advantage of avoiding both the risks and the long-term complications of a corneal transplant, such as the development of glaucoma and the progressive endothelial cell loss reported after endothelial keratoplasty.12,13 Future transplant surgery with Descemet membrane endothelial keratoplasty or Descemet stripping automated endothelial keratoplasty is still possible should it be needed after an unsuccessful Descemet stripping only. The intracameral injection of gas used during these keratoplasty procedures has been reported to cause opacification in hydrophilic intraocular lenses in some cases, but this has not been reported to occur in silicone lens materials, as is found in light adjustable lenses.14,15
When combining corneal- and lens-based procedures, consideration should be given to the fact that refractive outcomes after combined corneal- and lens-based surgeries are less predictable.16 One option would be to first perform the corneal surgery and, after stability is achieved, then perform cataract surgery at a later date. Although this option may improve the final refractive outcome, it carries the additional risk and inconvenience to the patient of having two surgeries and additional postoperative follow-ups. By using light adjustable lenses, these two surgeries can be combined, and if the refractive error requires correction, then this can be achieved with a minimally invasive light delivery system. Another advantage to only having one combined surgery instead of two separate surgeries would be less additional damage to the endothelium.17
Few articles have been published on the use of multifocal lenses combined with Descemet membrane endothelial keratoplasty.18,19 In our patient, we chose to avoid the potential challenges of multifocal vision given his young age. Multifocal lenses have been discouraged in patients with macular degeneration. There is a 25% risk of early age-related macular degeneration and an 8% risk of late age-related macular degeneration in patients older than age 75. Given the age of our patient, he has a nonzero risk of developing age-related macular degeneration in the future. Our patient chose Descemet stripping only given the advantages outlined above. However, Descemet stripping only can also be associated with a refractive shift of approximately 0.50 D hyperopia.20 To provide the patient with the best refractive outcome, we used a light adjustable lens in his surgery to help offset this risk.
The light adjustable lens was approved by the US Food and Drug Administration in 2017. Because the use of a hydrophilic intraocular lens should be avoided in a patient with the potential for future endothelial keratoplasty where gas may be used,21 this silicone-based lens is a good choice in patients with Fuchs endothelial dystrophy.22 The light adjustable lens has been successfully used in surgeries combining endothelial keratoplasty and cataract surgery. The advantage of this lens in these cases is that the lens can be adjusted after the surgery once the cornea has stabilized. It also provides some depth of vision, increasing the ability of the eyes to work together, which is different from traditional monovision (see Figure 4 for slit lamp view of light adjustable intraocular lens in mydriatic eye).
Patients maintain stable refraction and good visual acuity and have no intraocular-associated pathologies with light adjustable lenses. Cataract surgery with this lens is a safe method to achieve good vision without long-term complications.23 Silicone intraocular lenses have been safely used for several decades with no long-term complications, and so far, the silicone-based light adjustable lens has shown a similarly high safety profile.17 This light adjustable technology may also be helpful for other challenging patients, including those with prior radial keratotomy, ectasia, or other corneal irregularities.24 The light adjustable lens is contraindicated in patients with preexisting macular disease, prior history of herpes eye infection, and intake of medications that may increase sensitivity to ultraviolet light. Additionally, light adjustable lenses should not be advocated in patients with poor compliance to the postoperative schedule, as this lens requires additional light adjustments and lock-in treatments. Furthermore, patients must be compliant in wearing ultraviolet protective glasses until the final lock-in procedure is able to be performed.
The optics of the light adjustable lens contain light-sensitive silicone macromers. A few weeks after surgery, the refractive power of the lens can be changed by up to three diopters with ultraviolet irradiation from a light delivery device. At each treatment, the patient is fully dilated and placed at a light delivery device while the examiner holds a lens to the eye (see Figure 5). In cases of residual postoperative hyperopia, the central area of the lens is treated by ultraviolet light (365 nm), and in cases of residual postoperative myopia, the periphery of the lens is treated. Up to three adjustments can be performed, and each treatment generally lasts anywhere between 30 and 120 seconds. Finally, the refractive properties of the lens are fixed permanently with two final irradiation lock-in procedures.17 Light adjustable lenses can be removed if necessary. In this case, by combining Descemet stripping only with this modifiable light adjustable lens, additional surgeries are less likely for this patient.
CONCLUSION
Fuchs endothelial corneal dystrophy is the most common endothelial dystrophy, and current medical management is limited to topical hyperosmotic agents. Surgical intervention is often necessary when patients experience a reduction in acuity and quality of vision.25 Corneal transplantation is still a viable option, but newer surgical techniques such as Descemet stripping only may be recommended for patients with central guttata and a good peripheral endothelial cell count. Recovery after Descemet stripping only may take longer than traditional endothelial transplantation, but some advantages include no risk of rejection, no need for long-term immunosuppression therapy, and no need for graft tissue. Also, because it can be more difficult to predict a patient’s post–cataract surgery refractive outcomes when they also have Fuchs dystrophy, these patients may benefit from having a light adjustable lens implanted. Once refractive stability is achieved after surgery, a light delivery device may be used to change the shape, and thereby prescription, of the light adjustable intraocular lens. This can also provide a patient with subjective experiences to determine acceptance of monovision before finalizing the prescription. This case illustrates a very successful combined Descemet stripping only and cataract surgery with light adjustable lens implantation in a patient with Fuchs endothelial dystrophy.
No identifiable health information was included in this case report
TAKE HOME POINTS
-
Descemet’s stripping only may be an excellent surgical option for managing Fuch’s dystrophy, especially for patients with central guttata and a good peripheral endothelial cell count.
-
Because it can be more difficult to predict a patient’s post cataract surgery refractive outcomes when they also have Fuch’s dystrophy, these patients may benefit from having a light adjustable lens implanted.
-
Once refractive stability is achieved after surgery, a light delivery device may be used to change the shape, and thereby prescription, of the light adjustable intraocular lens.
-
Light adjustable lenses can also provide a patient with subjective experiences to determine acceptance of monovision prior to finalizing the prescription.