INTRODUCTION
Corneal allogenic intrastromal ring segments is a new technique to help improve the corneal shape of the keratoconic eye in an effort to improve a patient’s uncorrected visual acuity. Although the procedure is similar to intrastromal corneal ring segments, in which polymethyl methacrylate ring segments are implanted deep into the stroma, corneal allogenic intrastromal ring segments instead use donor corneal stromal tissue. Initially developed by Dr. Soosan Jacobs, the corneal allogenic intrastromal ring segments surgery has undergone changes in technique.1,2 A recent change was the introduction of the Istanbul nomogram and the use of sterile allografts (KeraNatural; Lions Vision Gift, Portland, Oregon, and Boston, Massachusetts). The following is a case report of the first patient within the United States who elected to undergo the corneal allogenic intrastromal ring segments procedure using KeraNatural and the Istanbul nomogram.2
CASE REPORT
A 54-year-old Asian Indian man with keratoconus presented to the clinic with a desire to make his prescription “more simplified.” He was diagnosed with keratoconus in the 1980s and has used glasses, corneal gas permeable lenses, and scleral lenses to correct his vision. The patient had a demanding work schedule that required him to work 20-hour days with contact lenses, and to compensate for this, his previous provider had recommended he alternate between two pairs of scleral lenses so that he could maintain comfortable vision during this time.
Per his previous doctor, his keratoconus had been stable for the past 10 years in both eyes. He was referred to the University Eye Institute for a corneal evaluation and to discuss various keratoconic treatment options, including corneal crosslinking and intrastromal corneal ring segments with synthetic segments. In addition to having keratoconus for nearly 40 years, his ocular history was also significant for cataracts and epiretinal membranes in both eyes. His medical history was significant for thyroid disease, hypercholesterolemia, and coronary artery disease, for which he was taking atorvastatin 20 mg and metformin 500 mg per day.
His entering, uncorrected visual acuity was 20/300 in the right and left eyes. His pinhole acuity was 20/100 in the right eye and 20/80 in the left. When corrected with contact lenses, his visual acuity improved to 20/30 in the right and left eye. Corneal topography demonstrated inferior cones, with right eye keratometry values of 47.4/50.1@110.3 with a maximum keratometry value of 51.7 diopters and left eye keratometry values of 48.6/51.7@58.5 with a maximum keratometry value of 55.1 diopters. Refraction was found to be -10.25 -4.50 × 030 in the right eye with a visual acuity of 20/60 and -10.25 -4.75 × 155 in the left eye with a visual acuity of 20/40. Slit lamp examination revealed corneal thinning and 2+ nuclear sclerosis cataracts in both eyes. Corneal allogenic intrastromal ring segments surgery was suggested as an option, and the patient opted to pursue the procedure, with the understanding that one eye would be performed at a time.
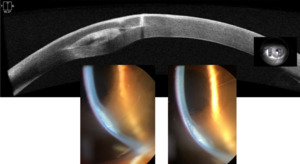
The patient underwent corneal allogenic intrastromal ring segment surgery using the Visumax 500 (Carl Zeiss Meditec AG, Jena, Germany). This laser centers the treatment on the patient’s visual axis. The following tunnel parameters were used: 4 mm inner diameter, 7.5 mm outer diameter, tunnel depth of 250 µm, and one incision at either end of the tunnel. A 495-µm-thick segment was inserted into the tunnel and trimmed to 160 degrees (Figure 1).
At his 1-day follow-up, the patient’s unaided visual acuity was 20/80-1 in the right eye (Figures 2 and 3). His corneal topography had flattened significantly centrally and steepened inferiorly in the mid-periphery outside of the ring segment, as expected. His keratometry values in the right eye had changed to 40.0/45.6@128.8. Over the next few weeks, the patient noted that his vision would fluctuate day to day, which was reflected in his manifest refraction. At the 1-week visit, the patient’s refraction was -4.25 -3.00 × 043 with a visual acuity of 20/60. At the 3-week follow-up appointment, the patient’s refraction was -1.50 -3.00 × 043 with a visual acuity of 20/100+2.
At his 2-month follow-up while wearing newly designed scleral lenses, his best corrected visual acuity was 20/50, and it was noted that his cataract had significantly worsened. The scleral contact lens fit was suspended, and it was recommended that cataract surgery be performed once his cornea stabilized. Over the next 3 months, his cornea continued to flatten and stabilize; however, his vision continued to deteriorate due to the cataract. The decision to pursue cataract surgery ahead of the 6-month corneal stabilization period was made as the patient was having difficulty reading text on his computer because of his cataract. Prior to cataract surgery, his cornea had stabilized to 38.2/45.3@126.7, demonstrating 9.2 diopters of flattening of the flat keratometry reading and 4.8 diopters of flattening of his steep keratometry reading.
One week following cataract surgery using a scleral tunnel technique, his uncorrected visual acuity improved to 20/70+2, and with a refraction of +0.50 -5.00 × 025, he was able to see 20/30+2. His spherical equivalent after cataract surgery matched the predicted outcome using the Barrett Formula to calculate his intraocular lens power. His cornea had further flattened to 36.9/44.1@122.2, increasing the total flattening achieved to 10.5 diopters (Figure 4).
Corneal epithelial thickness was measured with anterior segment optical coherence tomography. The average epithelial thickness in the area overlying the cone in the inferior cornea was 45 µm before corneal allogenic intrastromal ring segments surgery and 61 µm after the procedure. This demonstrated an average epithelial thickening of 16 µm over the now flatter cone. Central epithelium also thickened from 41 µm preoperative to 49 µm postoperative. The superior cornea showed relatively stable epithelial thickness of approximately 45 µm before and after surgery. The measured implant thickness was 532 µm at 6 months.
Five weeks following cataract surgery, the patient returned for a scleral contact lens fit in the right eye. A topography of the patient’s sclera was performed, and a custom, free-form scleral lens design was ordered. A 17.0-mm-diameter scleral lens with a 7.67-mm base curve radius, 5130 µm sagittal depth, and -3.00 -1.25 × 175 lens power was placed on the patient’s eye. A fluid reservoir of approximately 200 µm was seen centrally with complete corneal clearance 360 degrees. The lens haptic aligned against the patient’s sclera with no blanching or impingement. The patient achieved a visual acuity of 20/20 and indicated excellent all-day comfort through the lens.
Three months after restarting scleral lens wear in the right eye, the patient reported that he had been using the scleral lens for an average of 12 hours per day. Although uncorrected, the patient felt that he could use his right eye for near tasks comfortably, which he had been unable to do prior to the corneal allogenic intrastromal ring segments procedure. The corneal allogenic intrastromal ring segment procedure provided him the option of not wearing his scleral lens when doing near tasks and while in his home environment. The patient is scheduled to have corneal allogenic intrastromal ring segment surgery with KeraNatural performed in the left eye followed by cataract surgery once the cornea is stabilized.
DISCUSSION
Corneal disorders and irregularities can severely impact an individual’s vision. The distorted and blurry vision caused by keratoconus can often only be corrected with contact lenses. Glasses are frequently not enough for useful vision. Patients with keratoconus rely heavily on contact lenses that, if worn for too long, can have negative side effects on the health of the eye.3
Intracorneal ring segments with synthetic inserts (commonly polymethyl methacrylate) have been used for keratoconus to improve vision; however, their popularity has been declining. The goal of intracorneal ring segments has been to reduce corneal asymmetry and steepness of the cone to improve spectacle visual acuity and unaided visual acuity in those with contact lens intolerance and to delay corneal transplantation. Studies have shown that approximately 85% of patients gain at least one line of uncorrected or best corrected visual acuity and will achieve, on average, 3 diopters of flattening, but many patients do not improve more than three lines of uncorrected or best-corrected visual acuity.4,5 Conversely, our patient achieved 10.5 diopters of flattening with corneal allogenic intrastromal ring segments. Patients with mild to moderate visual acuity at the time of synthetic ring implantation were more likely to lose lines of vision after the procedure.6 Postoperative complications that have been observed with intracorneal ring segments with synthetic inserts include ring segment extrusion, corneal neovascularization, corneal haze, segment migration, corneal melting, and infectious keratitis.6
Although various specialty contact lenses can be successfully fit over corneas with polymethyl methacrylate intracorneal ring segments, it can make the fit more complicated.7–9 With corneal gas permeable lenses, lens decentration is a concern. Knowledge of reverse geometry lens design is needed, and selecting larger lens diameters has been shown to be helpful.10 Additionally, corneal erosions over the inserts and severe corneal neovascularization have been documented with corneal gas permeable lens wear.11 Although scleral contact lenses have increased in popularity so that patients with even highly irregular corneas can wear lenses comfortably throughout the day,12,13 fitters must make midperipheral changes to mimic the oblate corneal shape of patients with intrastromal ring segments.
Corneal transplants can help with uncorrected vision and dependence on contact lenses but are associated with severe complications and need long-term care. In addition, the outcome is not guaranteed, and the eye is weakened in the process. An alternative to corneal transplants is corneal allogenic intrastromal ring segments surgery. First introduced by Dr. Soosan Jacob in 2018, it has the potential to improve a patient’s quality of life by offering improved vision and decreased dependency on contact lenses.1 Similar in principle to the intracorneal ring segment procedure, allogenic segments created from donor corneal buttons are used rather than synthetic segments.1
Corneal allogenic intrastromal ring segment surgery aims to correct corneal irregularities and improve visual acuity in patients. The surgery consists of inserting sterile corneal allograft segments/rings into the cornea, reshaping and restructuring the cornea.2 Because of this, the corneal allogenic intrastromal ring segments procedure is effective in treating conditions such as keratoconus and potentially post–refractive surgery complications that involve thinning of the cornea. Patients can experience improvement in visual acuity, enabling them to regain clearer vision with glasses.
Corneal allogenic intrastromal ring segment surgery is a minimally invasive procedure that offers several advantages over traditional corneal transplant techniques or the use of synthetic rings. Unlike full-thickness corneal transplant, the corneal allogenic intrastromal ring segments surgery involves the placement of allograft intrastromal segments/rings into the corneal layers without the need for large incisions, sutures, and exposure to the anterior chamber. This approach results in reduced trauma to the eye, faster recovery times, and less postoperative discomfort for patients. To date, because corneal allogenic intrastromal ring segments are sterile allografts made of corneal tissue and share the same refractive index of the host cornea, there have been no reports of corneal melt, foreign body sensation, and halo or glare effects that are commonly associated with the implantation of rings made out of polymethyl methacrylate.14 Additionally, no cases of allograft rejection have been reported.15
With this case report, we present the first use of KeraNatural in corneal allogenic intrastromal ring segments surgery in the United States. Dr. Jacob used regular corneal tissue for her procedures. In contrast to normal corneal tissue, KeraNatural sterile allografts have a 2-year room temperature shelf life and a sterility assurance level of 10-6. Fresh corneal tissue has a limited use time of only 2 weeks in cold storage and greater risk of bacterial and fungal contaminants.16 Additionally, when compared with the use of a fresh tissue that generally results in one transplant from one donor cornea, KeraNatural can restore sight to up to five recipients from one donor cornea, allowing for greater access to corneal tissue in areas of the world where limited availability to corneas exists.
One of the unique features of using KeraNatural for corneal allogenic intrastromal ring segments surgery is its ability to adjust and potentially reverse the procedure to suit individual patient needs. Although synthetic implants such as INTACS (Addition Technology, Lombard, Illinois) only come in 150-degree arc lengths in six thicknesses between 210 µm and 450 µm,17 there is an unlimited number of ways in which implanted corneal tissue can be modified. Conversely, the length of the allograft rings can be adjusted in the operating room by the surgeon to affect the outcome of the procedure. Because corneal tissue is soft and pliable, unlike synthetic rings that will never change size or shape, the tissue will always be impacted by the size of the tunnel it is placed into and will integrate and create a fusiform shape resulting in a more normal corneal surface.
Currently, there are limited data regarding the reversibility of allogenic ring segments; however, it is expected that, similar to synthetic ring segments, allogenic ring segments can be removed or replaced accordingly if a patient’s condition changes. Approximately 10% of keratoconic eyes managed with synthetic ring segments need to have the ring segments adjusted, often with good results.18 Encouragingly, patients who had their synthetic ring segments replaced with corneal allogenic ring segments after anterior stromal necrosis avoided stromal thinning and experienced better visual outcomes compared with eyes that had the synthetic ring explanted.14
The corneal allogenic intrastromal ring segments surgery offers a safer alternative to traditional corneal transplant and synthetic intrastromal ring techniques. By avoiding full-thickness transplants and synthetic alternatives, the risk of complications such as graft rejection/failure, corneal melt, foreign body sensation, and glare are significantly reduced.19,20 Additionally, the minimally invasive procedure and use of terminally sterilized allografts lowers the risk of infection and postoperative inflammation.
Patients who undergo the corneal allogenic intrastromal ring segment procedure seem to experience faster recovery times compared with other corneal treatments. Because the surgery is minimally invasive, the healing process is typically quicker, and patients can return to daily activities sooner. In our patient, visual rehabilitation with KeraNatural for corneal allogenic intrastromal ring segment surgery was more rapid when compared with a corneal transplant.
As has been noted in previous studies, the corneal epithelium in keratoconic eyes usually thins over areas of relative increases in curvature. Because corneal allogenic intrastromal ring segments induces a relative flattening of the cornea, a thickening of the corneal epithelium may be observed postoperatively.21
CONCLUSION
Corneal allogenic intrastromal ring segments surgery represents an advancement in corneal treatments, offering individuals with corneal irregularities a chance to regain their vision and improve their quality of life. With its minimally invasive approach, ease of customization in the operating room, and faster recovery times, it provides a promising solution for patients seeking effective and safe treatment for corneal disorders. As this innovative technique continues to evolve, it holds the potential to reshape the landscape of corneal surgery and provide hope for those in need of vision restoration who now can only rely on contact lenses for their vision.
No identifiable health information was included in this case report.
Take Home Points
-
Corneal allogenic intrastromal ring segment surgery improves uncorrected visual acuity in keratoconus patients.
-
This procedure offers several advantages over traditional corneal transplant techniques or the use of synthetic ring segments.
-
Patients who undergo corneal allogenic intrastromal ring segment surgery are still able to be fit in contact lenses and achieve excellent visual outcomes.