INTRODUCTION
Aniseikonia, from the Greek terms an meaning “not,” is meaning “equal,” and eikon meaning “image,”1 is a condition where the two eyes view relative differences in size or shape.2 There are four types of aniseikonia most recognized in the literature: physiological aniseikonia, neurological aniseikonia, optical aniseikonia, and retinal aniseikonia.2 Physiological aniseikonia arises from ocular images coming from 2 different vantage points, enabling stereopsis.2 Neurological aniseikonia is thought to be part of normal cortical processing that allows for tolerance to small amounts of aniseikonia.2 Optical aniseikonia is caused by refractive components external to and internal to the eye.2 Retinal aniseikonia is from anatomical disruption of the photoreceptors’ distribution,2 commonly due to conditions such as epiretinal membrane, macular hole, macular edema, macular degeneration, and retinal detachment.3 Optical treatments—contact lenses, contact lens-spectacle combinations (Galilean or reversed Galilean telescope), and iseikonic lenses—alter overall magnification but may not fully address nonuniform retinal aniseikonia.
This report presents a case of epiretinal membrane-induced aniseikonia with minimal refractive error after cataract extraction. Treatment with iseikonic correction and slab-off improved symptoms. Adding a bifocal design further enhanced function and patient satisfaction. No identifiable health information was included in this case report.
CASE REPORT
Initial Visit (Visit #1)
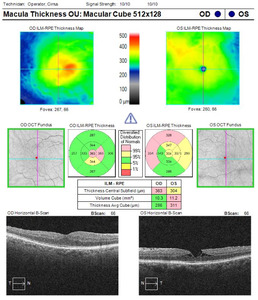
A 61-year-old man presented to the binocular vision clinic with symptoms of macropsia in the right eye after receiving a membrane peel 1 year prior to examination and cataract surgery 2 months prior to examination. He had been diagnosed with a lamellar hole in the left eye, contributing to left eye micropsia (Figure 1). No ocular surgeries had been performed. He subjectively estimated that the image was approximately 10% more vertically magnified in the right eye and reported constant vertical binocular diplopia as well as worsened depth perception. This significantly impacted his enjoyment of activities such as hiking, biking, fly fishing, and skiing. His medical history was noncontributory.
The results from Beren’s 3-figure Worth Light test demonstrated fusion at all distances and lighting conditions. The Randot Stereotest (Stereo Optical) revealed 50 seconds of arc local stereopsis but no global stereopsis. Pupils were equal, round, and reactive and had no relative afferent pupillary defect. Extraocular motilities were full in both eyes. Visual acuity was 20/20 in each eye through the habitual correction of right eye +1.00 -1.25 ×078 2∆ base-out and left eye +1.50 -1.50 ×107 1.5∆ base-out and 0.5∆ base-down (verified through lensometry). Confrontation fields were full. The subjective refraction at distance revealed right eye +0.25 -0.50 ×180 (20/20) and left eye +1.25 -1.00 ×104 (20/20). A cover test through the subjective refraction in a trial frame revealed orthophoria at distance and 2∆ of exophoria at near. Vertical Maddox Rod at distance and near revealed 1∆ of right hyperphoria. The (Awaya) New Aniseikonia Test presented at 40 cm demonstrated 5% vertical magnification and 1% horizontal magnification in the right eye.
The patient was asked to return in 2 weeks for continued testing and lens demonstrations.
Visit #2
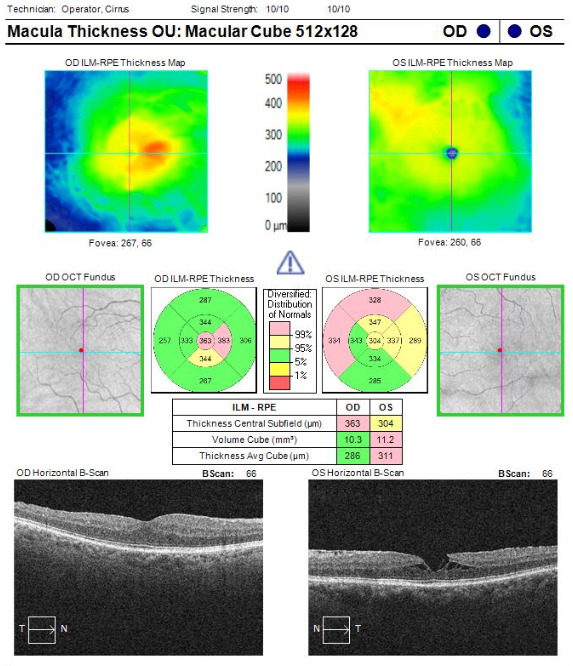
The goal of determining a combination of refractive correction and minimum iseikonic correction that would achieve acceptable visual comfort was conveyed to him prior to trialing lenses. Repeat refraction revealed slight changes to the subjective refraction in the right eye and no change in the left eye: right eye plano -0.75 ×180 (20/20) and left eye +1.25 -1.00 ×104 (20/20). The new manifest refraction with 1∆ base-down prism in the right eye was trialed in freespace, confirming improvement in clarity and depth perception. The myopic shift in the right eye had the fortuitous benefit of minifying the right eye image. In the left eye, a 2.75% overall magnification size lens was the minimum amount of correction that mitigated the aniseikonia when viewing with both eyes open. The New Aniseikonia Test presented at 40 cm measured a decrease in vertical magnification to 1% in the right eye. The Aniseikonia Inspector (version 3.5c) was subsequently used with the tentative spectacle prescription to assess the perceived magnification differences with varying target sizes (Figure 2).
It was recommended to order distance single-vision glasses to start. A prescription was released for right eye plano -0.75 ×180 1∆ base-down and left eye +1.50 -1.00 ×104 with 3% relative magnification. The patient preferred Trivex lenses for shatter resistance. He was educated on expectations regarding potential cosmetic factors, such as the lens being thicker in the left eye and recommended to choose zyl frames with a smaller lens size, ideally circular, to reduce weight and thickness differences in the lenses and improve wearability. The goal of improving, not eliminating, image size differences between the eyes was emphasized. He was asked to return at least 2 weeks after receiving the glasses.
Information such as the prescription, relative magnification needed, monocular distance, interpupillary distance, and his preferred lens material was provided to the specialty laboratory. Upon discussion with the optician and receiving lens parameter calculations from the specialty laboratory, it was possible to achieve 3.5% magnification using Trivex and a vertex distance of 13 mm in each eye. An order was placed based on these parameters: base curves of +3.00 and +6.50 and center thicknesses of 2.0 mm and 4.0 mm, for the right and left eyes, respectively. The pantoscopic tilt of the frame was measured to be 5°, and the frame wrap angle was 4°.
Visit #3
After trying to adapt to the glasses for 2 weeks, he felt his vision remained uncomfortable. If he viewed downward from the lens center (ie, visually scanning his environment, navigating stairs), he experienced a nauseating vertical binocular diplopia. He also reported that his right eye vision had changed gradually since the last visit and that the glasses provided little improvement in terms of size and depth perception.
The lenses were confirmed to match the specified power, base curve, center thickness, and interpupillary distance. His entering distance and near visual acuities were 20/20 in each eye. The New Aniseikonia Test was repeated, revealing a perceived relative magnification of 4% in the right eye horizontally and 2% in the right eye vertically. The cover test demonstrated orthophoria at distance and 2∆ exophoria at near. The distance subjective refraction showed small changes in both eyes: right eye plano -0.50 ×135 and left eye +1.25 -1.00 ×104. The vertical Maddox rod test at near in primary gaze revealed no vertical deviation. However, when he was asked to look downgaze to a point where things appeared diplopic (~10 mm below the optical center), 3∆ of right hypodeviation was measured. An estimate using Prentice’s rule showed approximately 0.75∆ of base-down prism in the right eye, indicating a total of 1.75∆ of base-down prism in the right eye if accounting for the ground in prism as well. In the left eye, approximately 1.5∆ of base-up prism was estimated (using +1.50 along the 90° meridian to estimate rather than at 104°). The vertical prism induced between the two eyes summed up to be approximately 3.25∆ base-down in the right eye, or base-up in the left eye, which corresponds to the 3∆ of right hypodeviation measured using vertical Maddox rod. He was asked to bring out his cellphone and demonstrate the position and viewing distance at which he would typically look at his phone. Using a lens marker, the centers of his pupils were marked at this viewing location on the lens, and the total relative prism measured between these 2 points was 2.5∆ of base-up prism in the left eye.
He also often needed to look down at his watch or his phone for personal and work needs. A near add of +2.00 was accepted at his preferred cellphone and wristwatch viewing distance. The monocular interpupillary distance was confirmed, and segment height was measured using the same frames previously used.
He was advised to return 2 weeks after receiving the new glasses for follow-up.
An inquiry for the maximum achievable magnification was made to the optician at the laboratory, as the patient still had concerns with the amount of improvement of perceived aniseikonia with the last iseikonic lenses. Based on the materials available at the laboratory, it was possible to achieve 7% relative magnification in the left eye. The material and vertex distances would remain as Trivex and 13 mm in each eye. In the right and left eyes, the new base curves were +4.00 and +8.25 and the center thicknesses were 2.0 mm and 8.7 mm, respectively. The pantoscopic tilt and frame wrap angle were left unchanged. The glasses were sent back to the laboratory to be remade.
Visit #4
The patient expressed that he felt very happy with his vision with the most recent glasses. Although it was “imperfect,” the vision was much better. His entering distance and near visual acuities were 20/20 in each eye. The distance and near cover test results were orthophoria. Vertical Maddox rod testing also revealed orthophoria at distance and near both in primary gaze and in downgaze.
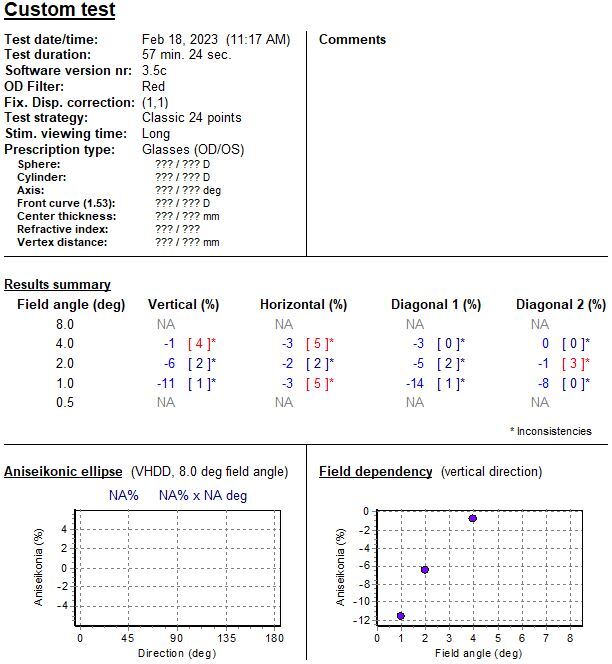
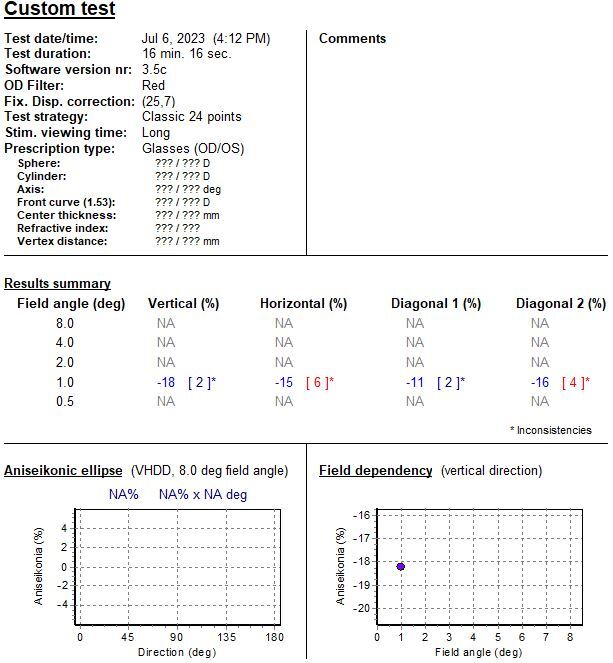
The New Aniseikonia Test was repeated, showing 0% magnification differences vertically and 1% magnification horizontally in the right eye. The Aniseikonia Inspector was used to measure the aniseikonia using varying target sizes, demonstrating overall improvement in aniseikonia (see Figures 2, 3, and 4).
Visit #5
Eleven months after the most recent visit, he returned for an annual eye examination seeking an additional computer single-vision prescription. Lensometry showed that his habitual bifocal correction matched the spectacle prescription prescribed at visit #3. His entering distance and near visual acuities were 20/20. Pupils and extraocular motilities were stable. Beren’s 3-figure Worth Light test results continued to demonstrate fusion at all distances and lighting conditions. Local stereo testing improved to 20 seconds of arc (from 50 seconds of arc). His global stereopsis improved from none previously to 250 seconds of arc. Although his refraction revealed a 0.50D hyperopic shift in the right eye—right eye +0.50 -0.50 ×135 and left eye +1.25 -1.00 ×104—no appreciable improvement in vision was demonstrated on the freespace trial. Therefore, the hyperopic change was not prescribed. A computer add of +1.50D was determined over the distance spectacle prescription from his habitual bifocals to provide the best clarity for his preferred working distance.
DISCUSSION
Common symptoms of aniseikonia include asthenopia, headaches, metamorphopsia, nausea, vertigo, dizziness,1,3,4 and horizontal/vertical diplopia. Vertical diplopia is common in retinal aniseikonia due to decompensated vertical strabismus or from central-peripheral rivalry.5 The latter arises from a mismatch between central and peripheral sensory fusion secondary to the epiretinal membrane disproportionately impacting macular photoreceptor distribution. Shipman et al described this phenomenon as “macular diplopia”6 and DePool et al referred to this as “dragged-fovea diplopia syndrome.”7 Dynamic aniseikonia, an effect of Prentice’s rule, can cause vertical diplopia when looking above or below the optic center. Anisometropic spectacle wearers experience increasing vertical prism with downgaze, challenging their limited vertical fusional range.
In retinal disease, macropsia arises from macular contraction and photoreceptor structure condensation.8–10 Among other retinal pathologies, epiretinal membranes tend to result in more severe aniseikonia symptoms.8 Even after membrane peel, acuity tends to improve more than aniseikonia.9,11 This may be because photoreceptor disruption persists despite restoration of overall retinal structure.8,12
There are various ways to quantify aniseikonia: the space eikonometer (the gold standard13 but now obsolete), the New Aniseikonia Test, and electronic tests such as the Aniseikonia Inspector. The Aniseikonia Inspector software measures aniseikonia up to 24% across the horizontal, vertical, and diagonal meridians, as well as varying target sizes. However, it is no longer being serviced. The New Aniseikonia Test is available, can be easily administered in-office, and exhibits good repeatability.14 However, it tends to underestimate the amount of aniseikonia14,15 and contains only 1 available target size. Our patient showed a 4% improvement on the New Aniseikonia Test despite a 7% designed magnification, presumably due to the test targeting more peripheral retina. With the Aniseikonia Inspector, smaller test targets revealed a higher amount of aniseikonia (Figure 2), consistent with another case report.16
The Aniseikonia Inspector confirmed residual aniseikonia (7%-17%) with iseikonic correction (Figure 4). Yet, stereopsis and fusion improved, and patient satisfaction was achieved. De Wit and Muraki, as well as Curie’s case reports, drew similar conclusions that fully mitigating aniseikonia was not necessary to improve visual comfort and relieve aniseikonia symptoms.9,16,17
Other clinical tests exist but require lenses with known magnification (size lenses) to neutralize the aniseikonia. The Turville test18 dissociates the eyes using a septum, and a horizontal line target is presented. If vertical aniseikonia is present, each eye will perceive unequal distances between the horizontal lines. The percent magnification required to make the lines equidistant determines the percent of vertical aniseikonia. In the Brecher test,19 a Maddox rod is placed over 1 eye, and 2 transilluminators are presented approximately 20 cm apart. The result is 2 lines perceived by the eye behind the Maddox rod and 2 lights from the transilluminators viewed by the other eye. If aniseikonia is present, it can be measured by determining the magnification required to equalize the distance between the 2 lights and 2 lines.
For retinal aniseikonia, monitoring for stability of aniseikonia precedes treatment. Then, a step-wise approach includes an updated monocular refraction, strabismus evaluation with prism prescription as needed to reduce binocular diplopia, and then aniseikonia testing. Our patient’s smaller (1°) target showed 11% aniseikonia, closer to his perceived 10% vertical magnification, than with the 2° target, which yielded 6%.
Optical treatment depends on refractive error and magnification needs. The magnification produced from a lens with a dioptric power of D at a vertex distance of h (in meters) is described by the power magnification formula:
Mp = 1/ 1−Dh
The lower the dioptric power of the lens, the less magnification it creates. Hence, minimal refractive error limits the benefit of contact lens use to mitigate aniseikonia. Magnification can be further adjusted by changing the vertex distance of the spectacle lens.
Galilean1,20 or reverse Galilean telescopes are options to magnify or minify images. Such telescope systems can be created by combining spectacle lenses with contact lenses. Typical considerations for contact lens candidacy are relevant here, including but not limited to the ability to insert and remove the lens, significant dry eye, allergies, risk of eye infection, and cost. The use of contact lenses was not considered for first-line treatment due to the patient’s preference for not wearing contact lenses and the increased complexity of the evaluation process.
In cases of low refractive error, there is a limit to how much the base curve and lens thickness can be manipulated. Iseikonic correction involves adjusting the lens’ front surface power/base curve (D), center thickness (t; in meters), and refractive index (n) as described by the shape magnification formula:
Ms =1/(1−tD/n)
High-index materials reduce the thickness and steepness of the surface curves.21 That is, a near-plano lens requires greater thickness and steeper base curves, which can lead to distortion and lens thickness asymmetry that may not be cosmetically acceptable to the wearer. It is worth noting that in contrast to refractive aniseikonia, where iseikonic correction reduces the magnification difference between lenses, retinal aniseikonia warrants amplifying the optical magnification difference.
There are ways to improve the wearability of iseikonic spectacles. A small lens size and circular frames help minimize weight differences between the lenses. Aspheric lenses would reduce optical aberrations. Plastic frames can better mask the lens edge than metal or rimless designs. The final spectacles ordered had plastic circular frames with no obvious asymmetry when viewed from the front (see Figure 5). Material, cost, and likelihood for remakes were discussed upfront to set expectations.
Slab-off (bicentric grinding) is warranted when vertical diplopia is experienced when gazing off optical center, often on downgaze. Base-down prism is incorporated into the most plus lens or base-up prism to the most minus lens. Since slab-off produces a visible line in the lens to which it is applied, a bifocal was ordered for cosmetic symmetry and improved functionality.
If optical correction fails to maintain binocularity, occlusion methods such as translucent tape,5 Bangerter occlusion foil,5 pupil occlusion contact lens, and patching can relieve diplopia.
CONCLUSION
Optical treatment of retinal aniseikonia in patients who have minimal refractive error can lead to treatment success using iseikonic correction. This case showed that partial correction was sufficient to improve visual clarity, comfort, and stereopsis. The use of slab-off and bifocal design helped mitigate diplopia on downgaze and improved the functionality of the spectacles.
AUTHOR DISCLOSURES
The authors declare that they do not have any conflicts of interest or funding sources to disclose.