INTRODUCTION
Epidemic keratoconjunctivitis is a severe form of viral conjunctivitis that causes inflammation of the conjunctival and corneal tissue and most often results from human adenovirus.1 Adenovirus species D types 8, 37, and 64 (formerly known as 19a) are the most common causative serotypes,1 with newer serotypes 53, 54, 56, and 85 emerging in the literature.2,3 The predominance of species varies depending on the geographic location.2 Epidemic keratoconjunctivitis is highly contagious and has a long course of infection. It can survive in the environment because of its strong resistance to desiccation, remaining infectious anywhere from 10 to 30 days depending on the porosity of the surface.4 There are limited effective treatment options to shorten the duration of infection, resulting in significant health care costs and socioeconomic burden.5
Epidemic keratoconjunctivitis is primarily a clinical diagnosis, as laboratory confirmatory tests are not widely available in practice, and in-office point-of-care tests are not always reliable.6 Common clinical features include follicular and membranous conjunctivitis, preauricular lymphadenopathy, corneal subepithelial infiltrate formation, and corneal superficial punctate keratitis.1,6,7 Symptoms are varied but often more severe than other forms of viral conjunctivitis.1 Patients complain of chemosis, photophobia, epiphora, redness, and foreign body sensation.6 The condition typically starts unilaterally, with the fellow eye being affected in 70% of patients.8
Corneal involvement distinguishes epidemic keratoconjunctivitis from other adenoviral conjunctivitis cases because of the virus’ unique ability to penetrate the corneal epithelium.7 The delayed formation of subepithelial infiltrates is well known with epidemic keratoconjunctivitis,1–3,6,7 but the presence of corneal epithelial defects has been infrequently reported.9–12 This unique clinical sign was identified in 3 patients at the Illinois Eye Institute in Chicago, Illinois, over 2 years. This case series reviews the suspected pathophysiology of their development and how to treat epidemic keratoconjunctivitis in the presence of a corneal epithelial defect. No identifiable health information was included in this case report.
CASE REPORTS
Case #1
A 40-year-old African American woman was referred for evaluation of a red right eye that had persisted for 5 days and spread to the left eye the morning of the examination. Symptoms in the right eye included eye pain and foreign body sensation. She also reported mild systemic nasal congestion for 6 days with no fever. She was not a contact lens wearer, denied having contact with anyone with a red eye, and denied experiencing trauma. Her medical, ocular, and family histories were noncontributory. She was taking 1 drop of tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension 4 times a day in both eyes, which was prescribed by the referring provider, with only mild improvement in her symptoms. Her uncorrected distance visual acuity was 20/20 in both eyes. All entrance tests were within normal limits. Anterior segment evaluation showed signs of bilateral adenovirus conjunctivitis, which were worse in the right eye than the left, including 3+ diffuse bulbar conjunctival injection and chemosis, 2+ palpebral conjunctival follicular reaction, and serous discharge. No pseudomembrane was observed. Both corneas were clear, and anterior chambers were deep and quiet. Intraocular pressures were measured at 19 mm Hg in the right eye and 18 mm Hg in the left eye by Goldmann applanation, and undilated posterior pole evaluation was unremarkable in both eyes. The QuickVue Adenoviral Conjunctivitis Test (Quidel) results were positive. A povidone-iodine 5% ophthalmic solution irrigation was recommended in both eyes, but the patient declined. She was directed to continue taking 1 drop of tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension 4 times a day in both eyes and start taking 1 drop of preservative-free artificial tears every hour in both eyes. She was educated on the contagious nature of her condition as well as the importance of copious handwashing and preventive spread measures, and she was instructed to return in 10 days for a follow-up examination.
She presented 2 days later with complaints of worsening symptoms in the right eye. Her symptoms in the left eye were stable. She denied experiencing trauma or rubbing her eyes. Her best-corrected vision in the right eye had reduced to 20/30 and was stable in the left eye at 20/20. Pertinent new findings in the right eye included 1+ upper and lower eyelid edema and a large, superficial central corneal epithelial defect, measuring 4.5 mm horizontally and 5 mm vertically, that was stained with sodium fluorescein. Pertinent new findings in the left eye included a pseudomembrane on the left lower palpebral conjunctiva. There were no corneal infiltrates in either eye.
The pseudomembrane was peeled on the left lower palpebral conjunctiva without complications. A povidone-iodine 5% ophthalmic solution irrigation was performed in the left eye but deferred in the right because of the corneal defect. She was initially treated with supportive therapy in the right eye, which included the discontinuation of using tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension and the addition of 1 drop of polymyxin B sulfate 10 000 unit-trimethoprim 1 mg/mL solution 4 times a day. She was followed daily and had stable visual acuity, stable symptoms, and unchanged signs in both eyes. Given that there had been minimal improvement in the size of the corneal defect after 4 days, a silicone hydrogel extended-wear bandage contact lens was applied (lotrafilcon A, Air Optix; Alcon). The epithelial defect resolved 4 days later, and the bandage contact lens was removed without complication. At this point, 10 days after initial presentation, the patient had developed peripheral subepithelial infiltrates in both eyes. She was treated with 1 drop of tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension 4 times a day in both eyes. The patient was kept on this medication instead of being switched to a topical corticosteroid because she had a large supply of this medication remaining. Her remaining symptoms and corneal infiltrates resolved without residual scarring 3 weeks after initial presentation. She was successfully tapered off all medications, and her visual acuity returned to 20/20 in both eyes uncorrected. Refer to Table 1 for a treatment summary for all 3 patients.
Case #2
A 21-year-old Hispanic man presented with redness of the left eye that started 2 days prior to the examination and had spread to the right eye 1 day prior to the examination. Associated symptoms included sharp pain, watery discharge, photophobia, and progressively worsening blurred vision that was more severe in the left eye than the right eye. He was not a contact lens wearer, denied having contact with anyone with a red eye, denied having any recent illness or trauma, and denied rubbing his eyes. His best-corrected distance visual acuity with pinhole was 20/25 in the right eye and 20/60 in the left eye. All entrance tests were within normal limits. Anterior segment evaluation revealed presumed bilateral epidemic keratoconjunctivitis characterized by palpable preauricular lymphadenopathy, 3+ diffuse bulbar conjunctival injection, 3+ palpebral conjunctival follicular reaction, and pseudomembrane formation of the left eye more than the right. The left cornea had a large epithelial defect that measured 6 mm horizontally and 5 mm vertically (Figure 1A). There were no subepithelial infiltrates present on either eye, and the anterior chambers in both eyes were deep and quiet. Intraocular pressures measured at 15 mm Hg in the right eye by Tono-Pen (Reichert), and measuring was deferred for the left eye. The QuickVue Adenoviral Conjunctivitis Test results were negative. Dilated fundus examination was deferred at the initial visit but was unremarkable in both eyes when completed at the follow-up examination.
The pseudomembrane was peeled from the right and left lower palpebral conjunctiva without complications. A povidone-iodine 5% ophthalmic solution irrigation was performed in the right eye but deferred in the left because of the corneal defect. Topical treatment was initiated using 1-cm strips of erythromycin ophthalmic ointment 0.5% that were applied 4 times a day in the left eye, 1 drop of neomycin-polymyxin-dexamethasone 3.5 mg/mL-10 000 unit/mL- 0.1% ophthalmic suspension taken 4 times a day in the right eye, 1 drop of preservative-free artificial tears taken every hour in both eyes, and 1000 mg vitamin C taken daily.
The patient was followed closely for 10 days. Three days after initial presentation, the patient’s epithelial defect on the left eye had resolved (Figure 1B). The patient was instructed to discontinue erythromycin, start taking 1 drop of neomycin-polymyxin-dexamethasone 3.5 mg/mL-10 000 unit/mL- 0.1% ophthalmic suspension in the left eye 4 times a day, and continue all other medications as previously instructed. The patient’s symptoms resolved 10 days after initial presentation, and his best-corrected visual acuity returned to 20/20 in both eyes.
Case #3
A 35-year-old African American man was referred for evaluation of conjunctivitis in both eyes. He had complaints of redness, watery discharge, and itchiness in both eyes; however, the right eye was worse than the left. His symptoms started in the right eye, then spread to the left eye 8 days later. He was not a contact lens wearer and denied having trauma or recent illness. His medical, ocular, and family histories were unremarkable. He was taking an unknown antibiotic eye drop 4 times a day in both eyes and azelastine hydrocholoride 0.05% twice a day in both eyes, and both of these treatments were prescribed by the referring urgent care center. The patient showed no signs of improvement in his symptoms. His best-corrected distance visual acuity with pinhole was 20/30 in the right eye and 20/25 in the left eye. All entrance tests were within normal limits. Anterior segment evaluation revealed bilateral epidemic keratoconjunctivitis characterized by 2+ diffuse bulbar conjunctival injection and chemosis, 2+ palpebral conjunctival follicular reaction, and pseudomembrane formation on the right lower palpebral conjunctiva (Figure 2). Additionally, the right cornea had a large, central, superficial epithelial defect (Figure 3A). There were no subepithelial infiltrates present on either eye, and the anterior chambers in both eyes were deep and quiet. Measurement of intraocular pressures was deferred in the right eye, and intraocular pressures were measured at 17 mm Hg in the left eye by Tono-Pen. The QuickVue Adenoviral Conjunctivitis Test results were negative, but epidemic keratoconjunctivitis was still the presumed diagnosis given the clinical signs.
The pseudomembrane was peeled and removed from the right lower eyelid without complication. A povidone-iodine 5% ophthalmic solution irrigation was deferred in both eyes because of the corneal defect in the right eye as well as the clinician’s preference to treat bilaterally. Treatment included 1-cm strips of erythromycin ophthalmic ointment 0.5% applied 3 times a day in the right eye, 1 drop of tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension taken 4 times a day in the left eye, 1 drop of preservative-free artificial tears taken every hour in both eyes, and 1000 mg vitamin C taken daily. Oral vitamin C was included for both case 2 and case 3 to promote corneal epithelial healing.13 The corneal defect resolved 3 days later. At that time, erythromycin was discontinued and tobramycin 0.3%-dexamethasone 0.1% ophthalmic suspension was added with the same dosing in the right eye because of the new presence of subepithelial infiltrates in both eyes. The patient was followed for the next month at various intervals. All symptoms and signs resolved, including the resolution of corneal infiltrates without any residual scarring, by the time of the 5-week follow-up examination. His best-corrected visual acuity returned to 20/20 in both eyes.
DISCUSSION
Epidemic keratoconjunctivitis presenting with geographic corneal epithelial defect is rare, occurring in 1.4% to 2.4% of cases.9,14 It was first reported in 1972 when Dawson et al identified 2 patients, out of 15 patients with adenovirus serotype 8 conjunctivitis, who developed large, central corneal erosions.10 Both patients were aged older than 60 years and had preexisting chronic ocular surface disease, which the author postulated may have contributed to the epithelial compromise.10 Our patients did not have significant comorbid ocular findings prior to presentation to support this claim. Both patients in Dawson’s report developed conjunctival pseudomembranes, just as all 3 patients in our series did, although not always in the same eye as the corneal defect. The authors concluded that corneal epithelial defect development, along with pseudomembrane formation in either eye, represents a more severe form of epidemic keratoconjunctivitis.10
Three additional reports have been published since the first, all supporting the evidence that corneal defects are unique to adenovirus serotype 8. In 1983, Darougar et al reported that 2 out of 82 patients with adenoviral conjunctivitis developed large epithelial erosions, compared with 72% and 43% who developed superficial punctate keratitis and subepithelial infiltrates, respectively.9 Both patients were confirmed to have adenovirus serotype 8 through laboratory testing.9 Chodosh et al described one patient who developed geographic corneal ulceration, along with conjunctival membranes, with laboratory-confirmed adenovirus serotype 8.12 Most recently, Lee et al reported 3 patients, all with polymerase chain reaction–confirmed adenovirus serotype 8 conjunctivitis, who developed large epithelial defects.11 A corneal defect can thus be considered a likely diagnostic sign of adenovirus serotype 8 conjunctivitis.9–12 Compared with other serotypes, serotype 8 causes more severe symptoms and a longer course of infection of epidemic keratoconjunctivitis.9 Recognizing a corneal defect as a marker for this serotype can assist clinicians when educating patients on the expected severity of their symptoms and anticipated timeline until resolution.
The specific serologies of our patients were unknown as laboratory confirmation via polymerase chain reaction viral sequencing is not widely used in conventional practice. Interestingly, 2 of our patients had negative test results on the in-office immunoassay screening test (now known as the QuickVue Adenoviral Conjunctivitis Test, formerly known as AdenoPlus). The diagnostic accuracy of this test has been variably reported since being first approved by the Food and Drug Administration in 2006, with sensitivity ranging from 40% to 93% and negative predictive values ranging from 71% to 99%.15–18 We suspect that the QuickVue tests yielded false negatives for the patients of case 2 and case 3 given that their clinical presentations strongly correlated with epidemic keratoconjunctivitis. It is also possible that differing techniques between providers or delayed timing of the test, leading to low levels of virus shedding in the eye,19 explains the negative results. The manufacturer recommends testing within 7 days of the first clinical signs,20 and the patient from case 3 presented shortly after this window. In cases like ours in which the in-office point-of-care testing does not align with the suspected diagnosis, a corneal defect may give the clinician additional criteria to help make a presumptive diagnosis.
The manifestation of a corneal epithelial defect occurs early during infection. Previous studies report onset between day 2 and day 9 after symptom onset.10,11 This aligns with the presentation of our patients, who developed their corneal defects 2 to 8 days after symptom onset. This lies in contrast to the well-documented later finding (14-21 days after symptom onset) of subepithelial infiltrate development.21
Multiple suspected pathophysiologies have been proposed for epithelial defect formation, but none have been proven. As mentioned previously, Dawson et al initially proposed that preexisting anterior segment disease precludes a patient to this finding,10 but this has been widely supported neither in subsequent literature nor by our case details. He also suggested erosions result from severe conjunctival inflammation, noting that all patients with corneal defects had conjunctival membranes.10 The fact that corneal defects presented before pseudomembranes in his report, and that the 2 findings presented in different eyes in case 1, rules this hypothesis out as the sole cause.10 The most likely theory, supported by several authors, is that adenovirus can directly infect corneal epithelial cells (versus simply replicating within the corneal epithelium).7,10,12 It is plausible a combination of the aforementioned factors leads to epithelial compromise, but further confirmatory studies are needed.
A corneal defect worsens a patient’s symptoms and complicates the treatment strategies for epidemic keratoconjunctivitis. Corneal epithelial defects, in isolation, are commonly treated with placement of a bandage contact lens.22 Using a contact lens in the setting of active ocular viral infection is generally contraindicated because of the risk of aggravating the condition and causing secondary coinfection, but forgoing a bandage lens on a geographic corneal defect will leave the patient in significant pain. One study exists that evaluated the use of silicon hydrogel extended-wear bandage contact lenses in 15 patients with varying forms of ocular surface abnormalities in adenoviral keratoconjunctivitis.23 The authors demonstrated the contact lenses offered almost immediate pain relief and caused no sight-threatening complications.23 Of note, all patients were treated with topical prophylactic antibiotics and were monitored daily.23 Our report highlights another example in which a bandage contact lens, in combination with prophylactic antibiotic therapy, was well tolerated with no side effects. Bandage contact lenses in conjunction with appropriate antibiotic coverage should be considered a viable treatment option for epithelial defects in epidemic keratoconjunctivitis, especially if the defects are persistent, large, and nonresolving as in case 1.
In-office irrigation with povidone-iodine is often used off-label to treat epidemic keratoconjunctivitis by reducing viral load and viral shedding and by shortening the course of infection.24,25 The administration of povidone-iodine into the eye causes significant symptoms of burning and stinging26 and would be poorly tolerated in an eye with a large corneal defect. Given that the presence of a corneal defect likely represents a more severe form of epidemic keratoconjunctivitis, povidone-iodine irrigation should be considered in a symptomatic fellow eye (without a corneal defect) to reduce symptom severity.
Topical steroids are used at varying times throughout a typical epidemic keratoconjunctivitis infection. In the acute phase, they may improve patient symptoms, but they have also been shown to increase viral shedding and delay viral clearance, therefore prolonging infection.27 When conjunctival pseudomembranes or corneal subepithelial infiltrates develop, topical steroids are prescribed because they are effective at reducing scar or symblepharon formation.1,27,28 With a corneal epithelial defect, steroids are used with caution because of their known side effects of delayed wound healing and potential bacterial superinfection.22 In an eye with an epithelial defect from epidemic keratoconjunctivitis, the benefit of steroid use may outweigh the risks, especially if corneal infiltrates or conjunctival membranes develop concurrently. Clinicians should use topical prophylactic antibiotic coverage in these cases.
CONCLUSION
Practitioners should consider the diagnosis of epidemic keratoconjunctivitis, specifically from adenovirus serotype 8, in the presence of severe conjunctivitis with geographic corneal epithelial defect. Insufficient evidence exists regarding the underlying pathophysiology, but it is thought to be due to preexisting anterior segment disease, severe conjunctival inflammation, and/or infection of the virus within the corneal epithelium. It typically presents within the first 9 days of symptom onset and resolves within several days without permanent visual sequalae if treated properly. An epithelial defect exacerbates symptoms, presents concern for secondary infection, and complicates the treatment options. Future research should focus on targeted antiviral treatments to reduce the duration of infection, improve patient outcomes, and reduce disease burden.
ACKNOWLEDGMENTS
We would like to thank Raman Bhakhri, OD, FAAO, for his mentorship.

_anterior_segment_photograph_at_initial_presentation_of_patient_2_left_eye_with_sodium_.png)
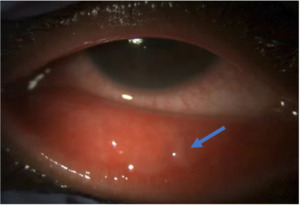
_anterior_segment_photograph_(10)_at_initial_presentation_of_patient_3_right_eye_showi.png)
_anterior_segment_photograph_at_initial_presentation_of_patient_2_left_eye_with_sodium_.png)

_anterior_segment_photograph_(10)_at_initial_presentation_of_patient_3_right_eye_showi.png)