INTRODUCTION
Currently, in the United States, epithelium-off cross-linking is the only US Food and Drug Administration–approved treatment to slow keratoconic disease progression. During this procedure, the corneal epithelium (the outermost layer of the cornea) must be removed.1 This creates a refractory healing period during which the epithelium must regenerate before contact lens wear can be resumed. Patients have been successfully fitted with rigid corneal lenses as early as 1 month after corneal cross-linking surgery, but a study by Sehra et al. used confocal microscopy to find that rigid corneal lens wear 3 months after corneal cross-linking had negative effects on corneal sub-basal nerve plexus healing, suggesting that the ideal time to be refit into lenses after corneal cross-linking may be uncertain.2 Theoretically, after the corneal epithelium is healed, a post–cross-linked cornea may be fit into most contact lens modalities, but if the patient needed rigid lens optics to restore vision prior to corneal cross-linking, they would likely need them postsurgically as well.
This case report will discuss the contact lens fitting and troubleshooting process in a patient with keratoconus after corneal cross-linking surgery. At the beginning of the fit, attempts were made to maintain the patient’s habitual rigid corneal lens wear to maximize health and longevity of wear. When this was unsuccessful, piggyback was also attempted unsuccessfully; this was followed by a pause in fitting to try to allow the postsurgical cornea to further stabilize. Ultimately, owing to the patient’s continued unstable and fragile cornea, which was not able to support contact lens bearing, the case culminated in a successful scleral lens fit, which vaulted the cornea completely.
No identifiable health information was included in this case report.
CASE REPORT
A 42-year-old Hispanic man with a history of bilateral, progressive keratoconus was referred to a local surgeon who recommended epithelium-off crosslinking surgery bilaterally, starting with his right eye. Although the patient was older than 40 years, an age at which it is thought progression should naturally stop,3,4 his ectasia had continued to progress. The patient had epithelium-off corneal cross-linking surgery on his right eye on March 1, 2023, and on April 11, 2023, he presented for a refit of his right contact lens after being given clearance from his corneal surgeon.
Before the surgery, the patient comfortably wore rigid corneal lenses in both eyes for 19 hours daily because of his need for visual correction. In 2023, he wore a spherical quad curve rigid corneal lens in the right eye and a spherical tricurve rigid corneal lens in the left eye based on Collaborative Longitudinal Evaluation of Keratoconus study design.5 He was fit into a quad curve design in the right eye in order to improve fit owing to his disease severity. Although, theoretically, aspheric lenses may help improve optics for patients with irregular astigmatism, lenses with multiple peripheral curves are thought to have a better fit for more advanced keratoconus.6
Overall, the patient had a history of good health, comfort, and vision with rigid corneal lenses despite his long hours of habitual wear. He found his vision in spectacles inadequate for work in construction and was highly motivated to be refit into lenses that he could wear comfortably for his habitual 19 hours of wear time.
The patient had an unremarkable systemic history and took no oral medications, and his last dilation on January 14, 2023, at our office was similarly unremarkable. His spectacle manifest on January 14, 2023, was as follows:
Right eye -13.50 -3.00 × 030 visual acuity 20/100
Left eye -13.00 -5.00 × 135 visual acuity 20/50
Given the extensive subsequent follow-ups, the case report hereafter will focus on right eye fit and summarize the most pertinent findings.
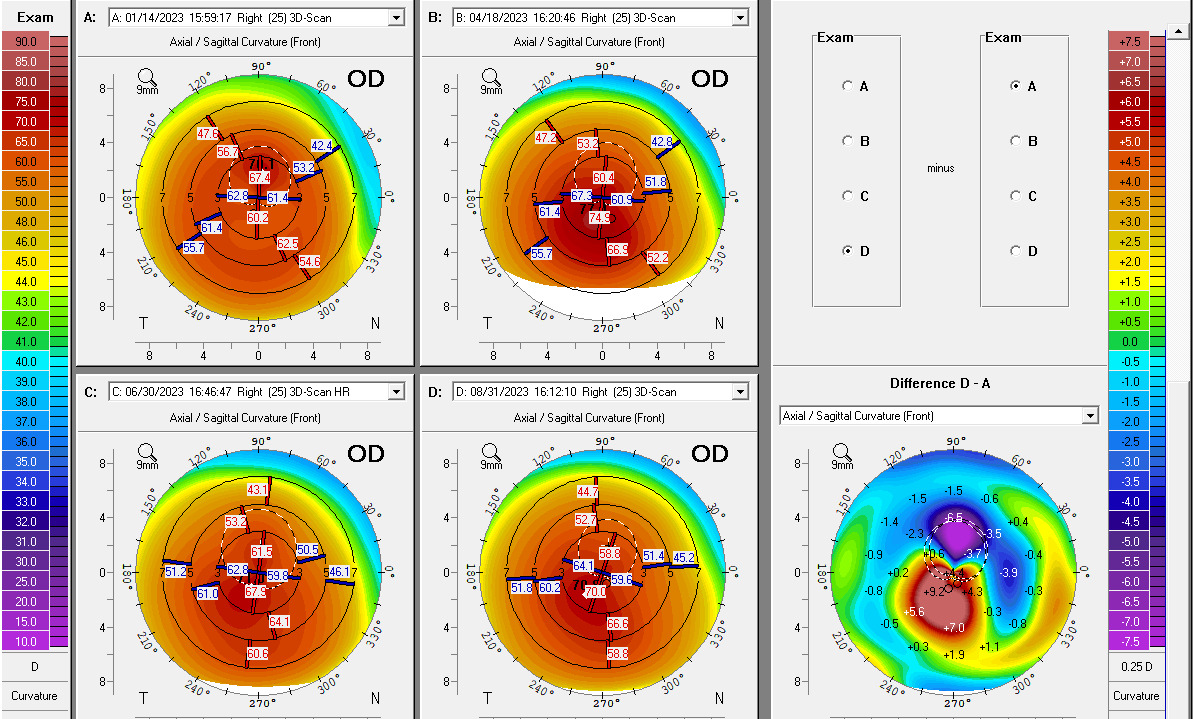
Notably, serial tomography was taken throughout the follow-up visits, revealing a changing corneal landscape and thickness. Figure 1 illustrates these changes.
Visit 1 (April 11, 2023): Rigid Corneal Fitting After Corneal Cross-Linking
The patient presented to the examination unaided in the recently cross-linked right eye (visual acuity: 20/300) and with his previously finalized corneal rigid lens in the left eye (visual acuity: 20/20-2). The patient reported that he no longer was using any drops in either eye and that his eyes felt comfortable.
New tomography images (Figure 2) were taken at this visit to determine corneal change after corneal cross-linking, and it was found that his right cornea was steeper and thicker than his presurgical values. The corneal cross-linking surgeon confirmed that given the patient’s thin cornea, it was necessary for them to swell the cornea using Photrexa to proceed with corneal cross-linking, and it was normal for the postsurgical cornea to be steeper immediately after the procedure.
Notable findings of the right eye included Fleischer’s ring, Vogt’s striae, 2-mm corneal scarring inferior to the visual axis, and trace pigment on the endothelium that was concentrated inferior-nasal to the visual axis. The anterior segment examination also revealed mild nasal and temporal pingueculae and 1+ papillae in the palpebral conjunctiva.
After anterior segment evaluation, the patient’s habitual right rigid corneal lens was applied for suitability of fit. At this visit, the quad curve rigid corneal lens (Optimum Comfort | 63.00 | -19.00 | 8.6 | 6.6 | 7.50 × 0.3 | 8.50 × 0.5 | 12.00 × 0.02 | gray | thin as possible) displayed moderate apical touch over the apex (blended to distinct borders of touch) fit with surrounding clearance, with a small bubble in the central clearance zone, mid-peripheral bearing, with average peripheral clearance 3 and 9 o’clock and maximum peripheral clearance at 12 and 6 o’clock. The patient saw 20/30- in the lens and did not have any over-refraction. Based on fit data, a 0.75D steeper lens was ordered, and the power was adjusted accordingly. The patient’s long hours of wear prompted continuation in a corneal rigid lens because it has superior tear and oxygen delivery compared with other modalities.7
The new Trial 1 lens order was as follows:
Optimum Comfort | 63.75 | -19.75 | 8.6 | 6.6 | 7.50 × 0.3 | 8.50 × 0.5 | 12.00 × 0.02 | gray | thin as possible.
Follow-Up Visit 2 (April 18, 2023): Initial Rigid Corneal Dispense
The Trial 1 lens was evaluated and dispensed, and the patient was educated to build up wear time and discontinue lens wear if he experienced any pain or irritation. The fit displayed a feathery apical touch and average peripheral clearance at 3 and 9 o’clock, had a small bubble in the mid-peripheral area of clearance, and was inferiorly decentered (however, when the lens was manually centered on the eye, the lens displayed apical clearance fit). The patient was able to see 20/30- with a plano over-refraction. Because the new lens displayed a feathery apical touch pattern on the cornea, a 0.50D steeper lens was ordered for possible dispense at follow-up, with the goal for a feathery apical clearance fit.
The Trial 2 lens order was as follows:
Optimum Comfort | 64.25 | -20.00 | 8.6 | 6.6 | 7.50 × 0.3 | 8.50 × 0.5 | 12.00 × 0.02 | gray | thin as possible.
Follow-Up Visit 3 (April 25, 2023): Rigid Corneal Lens Follow-Up, Fitting Into Piggyback
The patient presented to the office without wearing his right lens but reported he had worn the lens earlier that day for several hours. Upon evaluation of the patent’s right cornea, a circular impression ring that stained positively with sodium fluorescein was apparent.
The residual staining pattern suggested that there was lens binding; however, at the last evaluation, there was good movement on blink with an appropriate peripheral system. Given that the history of the fit was adequate, yet his cornea showed signs of superficial disruption, along with the evidence of instability of the corneal shape and remodeling by topography (see Figure 1), a soft piggyback fit was introduced so that the fit would not be as reliant on a stable corneal shape and the corneal epithelium would be protected from mechanical friction.
Ultimately, between the Trial 1 and 2 rigid lens, the Trial 1 with the piggyback soft lens had the best fit and was ultimately dispensed, as Trial 1 and the soft lens had good independent movement when evaluated. The Oasys 1-Day lens was chosen because of its daily modality for ease of use, moderate modulus (0.72), and high Dk (103). The patient was counseled on proper lens handling and hygiene.
Follow-Up Visit 4 (May 2, 2023): Piggyback Follow-Up
The patient returned wearing his piggyback lens system after 12 hours of wear that day. Despite confirmed appropriate rigid lens cleaning with Boston Simplus, good comfort, and a stable fit compared with the last visit, after lens removal, there was the presence of 2+ coalesced central corneal superficial punctate keratitis and a circumferential lens imprint negative stain with diffuse staining surrounding the imprint.
The severity of the sequalae from lens wear did not match the appropriate fit of the lenses, and the thought was the cornea was not yet stable enough to support a lens that sits directly on the cornea after corneal cross-linking. The recommendation was made to totally discontinue right lens wear for an additional month to allow further corneal stabilization before resumption of lens wear. The patient was further counseled to lubricate his right eye with nonpreserved artificial tears 4 times daily and to return to the clinic if he had any pain or irritation that was nonresolving.
Follow-Up Visit 5 (June 9, 2023): Redispense of Rigid Corneal Lens After 1-Month “Lens Break,” Now ~3 Months After Epithelium-Off Corneal Cross-Linking
No significant superficial punctate keratitis was present and the patient’s previous Trial 1 lens was applied and evaluated in office, and re-dispensed to the patient. The fit and the vision was the same as described in Follow-Up Visit 2.
Follow-Up Visits 6 (June 16, 2023) and 7 (June 30, 2023): Follow-Up for Rigid Corneal Lens
On June 16, 2023, the patient only wore the lens 20 minutes prior to the examination, and no sequelae was found. He was counseled to wear the lenses for several hours prior to the next corneal health check.
On June 30, 2023, the patient presented with reduced visual acuity (20/70+) that had no improvement with over-refraction. Evaluation revealed corneal staining secondary to rigid corneal lens wear, once more despite a seemingly adequate rigid corneal fit (feathery oval bearing centrally, surrounded by pooling and apical clearance with average peripheral clearance 12 and 6 o’clock, and minimum peripheral clearance 2 and 9 o’clock). The right cornea had an impression ring of the lens with negative staining surrounding the pattern of peripheral curves, and there was also 1-2+ circumferential staining in the midperiphery. The patient was asked once again to discontinue contact lens wear and use nonpreserved artificial tears 4 to 5 times daily.
The patient’s cornea had circumferential staining that appeared as if secondary to peripheral curve junctions. Subsequently, a third trial lens with heavy blending was ordered with an additional fifth peripheral curve to try to smooth out any harsh junctions between curves.
The Trial 3 lens order was as follows:
Optimum Comfort | 63.75 | -19.75 | 8.6 | 6.6 | 7.50 × 0.3 | 8.20 × 02| 9.1 × 0.3 | 12.00 × 0.02 | gray | heavy blend.
Follow-Up Visit 8 (July 21, 2023): Attempted Dispense of Rigid Corneal Lens With Heavily Blended Peripheral Curves, Beginning of Refitting Into Scleral Lens
After no lens wear in the right eye for several weeks, an attempt was made to dispense the previously ordered Trial 3 lens; however, the fit was inadequate because of decentration and a large central bubble. This lens base curve and optic zone was unchanged from Trial 2, so if the patient’s cornea had been relatively stable, there should not have been a drastic change in fit. Because of the unexpected poor fit and repeated corneal sequelae with and without piggybacking, it was discussed that refitting the patient into a scleral lens to vault the cornea would be most appropriate. Vaulting the cornea would circumvent fitting issues due to changing corneal shape and a seemingly fragile cornea. The patient agreed and scleral lens diagnostic fitting was completed using Alden Zenlens (Bausch and Lomb, Bridgewater, New Jersey). The patient was extensively counseled that he could not safely wear a scleral lens for as long as he wore his corneal lenses owing to limitations in tear exchange and oxygen.
A diagnostic fitting was performed, and from the evaluation, the Trial 4 scleral lens design was ordered:
Alden Zenlens Z3 Prolate| Boston XO2| -6.25| 7.1 BC|16.0 DIA| Sag: 4850| + 50 LC| Steep 1 by Flat 2.
Scleral Lens Finalization Visit Summaries
The patient was seen for follow-up visits on August 3, 17, and 31, 2023, to dispense, adjust, and finalize his scleral lenses. On August 31, 2023, an evaluation of the patient’s incoming right eye lens revealed 20/25 visual acuity (improved from 20/50 prior to corneal cross-linking) with a settled fit with thin but adequate central clearance. The thin tear clearance helped to maximize oxygen transmissibility and would be closely monitored with regular follow-ups; therefore, the lens was finalized (see Table 1 for full parameters and fit). The subsequent anterior segment evaluation revealed no active epithelial defects, rebound hyperemia, or any additional findings that were not found at his baseline examination in the right eye. The patient was asked to return for a health check in 3 to 4 months and was reminded of the importance of not wearing his lenses more than 8 hours daily. The patient reported compliance and that he wore his scleral lens for work, then removed the lens immediately afterward. The plan was to revisit the possibility of refitting into a rigid corneal lens after 1 year.
Another tomography image was taken at this visit for comparison with previous visits (see Figure 1). Overall, although the simulated K values were flatter than in April 2023, there were localized areas of central steepening up to 9.2D steeper than the patient’s curvature values immediately prior to surgery.
DISCUSSION
The corneal cross-linking procedure works to strengthen the covalent bonding between collagen fibrils in the cornea, improving biomechanical corneal stability and preventing corneal steepening.8,9 In the United States, the only currently US Food and Drug Administration–approved system available is the Epithelium-off Avedro Photrexa Viscous Photexra and KXL System (Waltham, Massachusetts). After corneal cross-linking surgery, the cornea may immediately steepen, but it will tend to flatten after 3 months compared with presurgical values.10 A retrospective study showed topography changed even 7 years after corneal cross-linking, with most patients’ corneas flattening, whereas 4.7% had comparative steepening.11 Notably, corneal pachymetry tends to thin after surgery, as in this case; however, corneal thickness tends to recover, with the exception that the thinnest pachymetry has shown to stay reduced relative to presurgical findings.12
After epithelial healing, patients may be able to tolerate contact lens wear as soon as 1 month following corneal cross-linking,13,14 but from the study by Mandathara et al., the average post–corneal cross-linking fitting time was 2.53 months.13 Although the patient was cleared for contact lens fitting 1 month after surgery, the patient’s anterior topography values continued to change even several months afterward, making finding an appropriate base curve lens difficult. Ultimately, it seemed his cornea was unable to handle the friction and bearing of normal rigid corneal or piggyback wear. Because the nerve plexus helps drive epithelial maintenance, and rigid corneal lenses impede sub-basal nerve plexus healing, this could be one mechanism that explains this case’s constant epithelial defects with rigid lens wear postsurgically.2 Perhaps the patient’s advanced presurgical ectasia and thin pachymetry contributed to making the postsurgical healing and corneal contact lens fitting journey atypical.
Ultimately, the patient was fit into a scleral lens, and although the comfort, corneal health, and vision provided with scleral lenses is extremely promising, there is very little tear exchange and oxygen availability to the cornea, and little is known about the long-term effects of the lenses on ocular health; therefore, patients fit into the scleral lens modality should be closely monitored.15–17 Studies show that post–corneal cross-linking corneas continue to change and remodel even years after surgery,2,11,18 so perhaps vaulting the cornea altogether with a scleral lens after corneal cross-linking is the most prudent fitting philosophy. On the other hand, it could be argued that lack of tear exchange and oxygen availability to the endothelium with scleral lenses could also delay healing.16,19
CONCLUSION
When prescribing contact lenses for patients after corneal cross-linking, even if the epithelium may be seemingly healed, not all corneas will be able to support all types of contact lenses, including lens modalities that were previously healthily worn. Although scleral rigid contact can vault corneal irregularity and help patients achieve excellent vision and comfort, little is known about the long-term effects on corneal health, and thus, monitoring is important. After corneal cross-linking, the corneal topography and biomechanics may continue to change; therefore, any contact lens fits should be closely monitored.